Preventative Dentistry
Preventative dentistry is the practice of caring for your oral health including your teeth. The goal is optimum oral health and preventing problems like
- cavities,
- gum disease,
- enamel wear,
- and more.

Initial Consultation
Initial Consultation / New Patient Check Up
The first people you will meet will be our friendly reception staff, who will ask you to complete a medical form.
Our dentist needs to be aware of your general state of health as this can often impact upon the condition of your teeth and gums and may effect medication such as anaesthetics and antibiotics we may use for you.
At your consultation you will have the opportunity to discuss any dental concerns you may have or how you would like your teeth improved.
Your dentist will give you a full oral assessment to help accurately plan which treatments would be best for the health of your mouth.
During this examination we will be looking at -

- Teeth and the way you bite, plus any missing teeth
- Original restorations – fillings, crowns, veneers etc.
- The health of your gums and surrounding bone around each tooth
- Your tongue, throat, cheeks and lips for signs of oral cancer
- Jaw joint evaluation
- Treatment planning
Dental X-rays will also be taken of your teeth to check for -
- Decay inside the tooth or between the teeth.
- Abscess or cysts on the roots of your teeth.
- Root positions
- Bone loss
Once the examination is complete, we will discuss the findings with you.
We will then create a treatment plan with alternative options for you, including all the benefits and risks of each procedure and the costings. This will allow you to decide what is best for your long term dental health.
Oral Hygiene
Oral Hygiene
Healthy Gums are:

- Pink in colour
- No areas of redness or inflammation
- No bleeding when brushing or flossing
- No tenderness or discomfort
In order to keep your gums healthy you need to remove the daily build up of plaque from all the surfaces of your teeth by:
- Brushing your teeth twice a day, for two minutes each time. Ask your dentist which type of tooth brush is best for you, as many of us use brushes that are too hard or too large.
- Floss your teeth, as a toothbrush doesn't always reach into the gaps in between the teeth or below the gum line.
- Do not brush your teeth too hard as this can damage your gums, ask your dentist or hygienist to show you the correct technique
- Use fluoride toothpaste.
If the daily build up of plaque is not removed, this can lead to the first stages of gum disease ‘Gingivitis’.
What is Gingivitis?

Gingivitis is caused by sticky bacteria which are known as ‘plaque’. Plaque collects in the small gaps between the gums and the teeth and if not removed by regular brushing and flossing will multiply by feeding on sugars found in your food and drink. This can lead to:
- Bleeding when brushing or flossing
- Soreness or discomfort
- Appear red in colour, puffy or swollen
Bleeding when brushing or flossing your teeth is the earliest and most common sign of gingivitis. Gingivitis is reversible if treated by a hygienist or by improved brushing and flossing techniques. However, if left untreated you will develop the later stages of gum disease, which is known as ‘Periodontal Disease’.
What is Periodontal Disease?
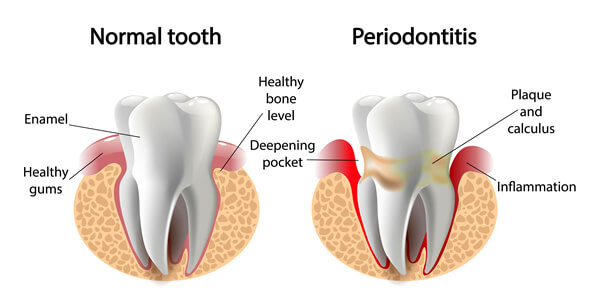
Periodontal Disease is the later stages of gum disease. This is when the bacteria infection under the gums progresses deeper and affects the bone and tissue supporting the tooth.
When suffering from periodontal disease, your gums will:
- Bleed when brushing or flossing.
- Will be red, swollen and tender.
- Bad Breath.
- The gum will have pulled away from the tooth, this is called ‘Pocketing’.
- Pus may be seen in the pockets around the tooth.

The infection damages the tissue that connects the gum to the roots of the tooth. Once the tissue has been destroyed the gum pulls away from the tooth, this forms a pocket which bacteria thrive in. If not treated, in time the bone anchoring the teeth in the jaw will resorb, making the teeth loose and eventually the teeth will fall out.
Periodontal disease is irreversible, but you can slow down the progression by regular visits to the Dentist and Hygienist as well as improving your oral hygiene at home.
Fluoride Treatments
Fluoride Treatments
Fluoride is a natural mineral found in food and water which helps to strengthen teeth and prevent tooth decay, by making the tooth more resistant to acid attacks from plaque and sugars. If fluoride is lacking from the diet, the teeth will be prone to tooth decay and cavities.
The hard outer surface of the tooth is called ‘enamel’, which contains mineral crystals. Everyday plaque bacteria and sugars in the mouth attack the enamel causing it to weaken. This process is called ‘demineralisation’. Minerals such as fluoride, calcium and phosphate from the food and water we consume and the toothpaste we use, helps to strengthen the enamel. This process is called ‘remineralisation’. Fluoride speeds up the remineralisation process.
Fluoride intake is very important when teeth are developing.
It can be taken into the body in two ways:
- The food and drink we consume or supplements.
- Fluoride toothpaste, mouthwashes or when applied directly to the teeth by the dentist or hygienist.
Fluoride treatments are offered to children who have a number of cavities or are at high risk of developing cavities. Adults can benefit too. Fluoride treatment is a very simple process administered by the dentist, dental therapist or dental hygienist which helps to prevent tooth decay.
Periodic Reviews
Periodic Examination / Reviews
The best way to maintain good oral hygiene is to brush and floss your teeth and to visit your dentist for regularly. Your dentist not only examines your teeth for signs of decay or damage, he also looks for early signs of gum disease and oral cancer.
It is normally recommended that you visit your dentist twice a year, although people who have severe gum disease or a weakened immune system may need to visit the dentist more often.
Your dentist will first ask if there have been any problems since your last dental check up and take a note of any new medication that you may be taking.
At your check up your dentist will:
- Check for early signs of decay or breakages
- Check existing restorations
- Look at your gums for early signs of gum disease – this will be done using a probe which is gently placed between the tooth and your gum to determine the stage of gum disease
- Examine your tongue, throat, cheeks & lips for signs of oral cancer
- Examine jaw joint evaluation
X-rays of your teeth are usually taken every year, unless your dentist notices a problem and needs an X-ray to look inside the tooth.
If cavities are found or your dentist feels that your oral hygiene needs to be improved, s/he will create a treatment plan outlining the work to be carried out and the costing; you will then need to make an appointment for the necessary treatment.
Occasionally, patients are referred to other dentists who specialise in the relevant fields of dentistry.
Snoring
Snoring
Snoring, like all sounds, loud or quiet, is caused by vibrations in the respiratory structures. It occurs during sleep when the area at the back of the throat or in the nose relaxes and narrows. The air movement is then restricted in the air passage, resulting in the sound.
There are many reasons for snoring some of which we can control –
- Being overweight and having excess fatty tissue around the neck.
- Smoking causes inflammation of the airways and irritates the nasal passages.
- Alcohol slows the brains responses causing more relaxation than usual.
- Medication, antihistamines and sleeping pills in particular, have the same effect as alcohol.
Some of which we cannot -
- Allergies which cause swelling of the nasal passages, Asthma, colds and sinus infections.
- Having a narrow throat, enlarged adenoids or a cleft palate all contribute to snoring.
- Ageing, middle aged men in general men have a wider neck and more soft tissue which causes vibration.
The most serious type of snoring can stop the breathing; this is called Obstructive SleepApnoea (OSA) and can be moderate to severe. In milder cases the airways narrow greatly but do not close. This results in breathing being very shallow loud snoring.
The more severe type of OSA is caused by the lack of muscle tone in the upper airway which causes the airway to close fully and one or more pauses in the breathing. The body’s natural reaction causes breathing again, with a gasp. It is a very difficult condition to diagnose and most people who have sleep apnoea don't know they have it, as it only happens during sleep. Your partner may be the first to notice the signs.
The main causes of Obstructive Sleep Apnoea
- Being overweight and having a lot of fatty tissue around the neck. However some people do have sleep apnoea who are not particularly overweight.
- Enlarged tonsils, especially in children.
Once sleep Apnoea is suspected a sleep study will be carried out to confirm the diagnosis.
How your dentist can help with snoring
There are many products on the market to help with snoring, but your dentist can fabricate a device that is custom made for you. It is called a Mandibular Advancement Device and works by holding your lower jaw and tongue forward therefore keeping your airway open whilst you sleep. Please speak to your dentist for further advice.
Sports Mouthguards
Sports Mouthguards

Mouthguards are made from a plastic material called Ethylene Vinyl Acetate (EVA).
EVA is strong and tough and can be easily moulded to fit precisely over your teeth and gums.
Mouthguards are the most effective protective pieces of equipment to help prevent injury to the mouth - protecting the teeth, lips, cheeks and tongue. A mouthguard does not only protect your mouth, it can also cushion blows to the mouth or jaw therefore preventing damage to the jaw, neck or brain.
Having a dentist take special impressions will create a guard to perfectly fit your mouth, teeth and gums, providing ultimate protection. The procedure is very simple; your dentist will take moulds of your teeth both upper and lower. They will be sent to the dental laboratory where our technician will fabricate your custom made guard.
Your sports mouth guard will need replacing over time. Just bring it along to your check-ups and your dentist will inspect it for wear and tear.
Teeth Grinding
Teeth Grinding

Teeth grinding is a surprisingly common occurrence and often happens whilst asleep. Most people are therefore unaware that they are grinding and only come to realise it when their partner complains of the noise the following morning.
Other noticeable effects of grinding (bruxism) are:
- Earaches
- Headaches
- Jaw pains
- Facial and neck pains
- Sleep disorder - both yourself and partner
- Sensitivity to hot and cold drinks
Why do we grind?
The most common reason for grinding is when we try and compensate for an imperfect bite. This is when the upper and lower jaw comes together but the teeth don’t seem to fit comfortably and you therefore try and force them into a perfect bite. Imagine chewing hard but with no food in your mouth.
You may also find that you suffer from jaw clenching which, if combined with grinding, will cause greater discomfort and damage to the teeth.
Stress can lead to grinding although you may be equally unaware that you are doing so as it often happens during your sleep.
What are the consequences of grinding?
As you try to compensate for the imperfect bite you end up biting harder and thus causing damage to the enamel on your teeth. It becomes a vicious circle as you bite harder to try and make the teeth fit better you end up creating more damage to your teeth by initially wearing down the tooth’s enamel to gradually wearing down the tooth itself.
What can be done about it?
- As most grinding occurs during your sleep, the most common solution is the use of a bite plate to prevent such grinding. This helps reduce the pressure of tooth grinding and helps prevent further damage to your teeth. Your dentist may also be able make adjustments to your teeth order to achieve a better bite and thus reduce the subconscious effort you are making.
- You can also get Botulinum Toxin treatment.
- Naturally, if your grinding is a result from stress then you should learn relaxation techniques and stress management.
Bad Breath
Bad Breath

Bad breath (or halitosis) is an unpleasant odour which can occur from time to time or be long-lasting.
We have millions of bacteria that live in the mouth, particularly on the back of the tongue and these bacteria feed on the food debris that accumulates in the mouth and between our teeth. The bacteria give off a sulphur compound and it is this that creates the bad odour. Smoking and drinking alcohol contribute to unpleasant odour. There are other conditions which affect the airways and stomach that can lead to bad breath too.
Improving your oral hygiene is the most effective way to eliminate bad breath. Brushing teeth and tongue twice a day using fluoride toothpastes, as well as flossing, will remove the bacteria which generally removes the odour.
Other things that help are:

- Drinking plenty of water
- Chewing sugar free gum after meals
- Stopping smoking
- Eating a well balanced diet
- Making regular visits to your dentist
The other causes of bad breath (which can be treated by your dentist) are:
- Infection of the gums ( Periodontal disease )
- Decayed teeth
- A condition called ‘Dry mouth’ affecting the flow of saliva
If your dentist finds that your mouth is healthy but you still have bad breath,
you may be referred to your family medical practitioner, as there are other causes of bad breath including
- Sinusitis and bronchitis.
- Problems within the stomach.
- Diabetes.
- Liver and kidney problems.